| Considering the coding complications with non-HIPAA-regulated entities |
THE GO-LIVE DATE for the ICD-10 conversion is fast approaching, and all HIPAA-covered healthcare entities should be working hard to be ready to go on October 1, 2015. The financial ramifications of the conversion are many, both in preparing for the conversion and once it has taken effect.
The United States is one of the last countries to convert to ICD-10 from ICD-9. “ICD-9 was developed in 1979. It is over 35 years old,” maintains Judy Monestime, an independent consultant and owner of PLM Consultants. As an American Health Information Management Association-approved trainer in ICD-10-CM/PCS, she has been following the conversion closely.
The U.S. uses ICD codes for billing and payments as well as the statistical tracking and evidence-based medicine it was originally meant for. “We’ve made lots of changes in healthcare. However, our classification system hasn’t revealed all of the changes we have made in our industry. The terminology has become outdated and obsolete; it’s not even the same terminology our doctors are using now,” explains Monestime. Consequently, the ICD-10 conversion will include upwards of 69,000 diagnosis codes for all providers (CM) and more than 79,000 procedure codes for in-patient procedures (PCS), while ICD-9 only used around 20,000 codes in total.
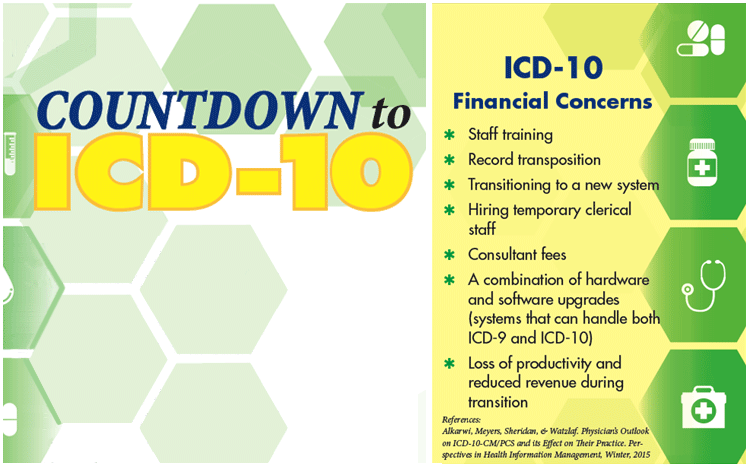
Financially, the conversion creates some definite challenges for providers. “The research does support that there will be some financial commitments,” Monestime explains, such as “your training, and working with your vendors if you have an EHR system, your Practice Management System,” she lists. “Also, just getting ready for understanding your work flow … and working with your payer to make sure that there aren’t any outliers that need to be addressed.”
Another point that also adds complexity to the conversion is the fact that ICD-9 codes will still be in use. For one, there will be those codes from September 30 and earlier that are still going through the system. “ICD-9 codes will be in use for at least a year,” Monestime points out. Additionally, there will also be the issue of non-HIPAA-regulated entities — such as auto, homeowner’s and worker’s compensation insurers — who don’t have to convert to ICD-10.
“Physicians will have to communicate with those non-HIPAA-covered entities to verify whether or not they are going to be transitioning; and if not, then they will have to continue to use the ICD-9 codes for those payers until they decide to switch.”
If not prepared by October 1, healthcare providers will definitely feel the financial ramifications. According to Monestime, “CMS — the Center for Medicare and Medicaid — has said that, on October 1, if a provider submits a claim that does not have an ICD-10 code, then those claims will be denied. They will not be processed.” Commercial payers historically follow CMS, so it’s likely that providers will not be able to get any payment for non-ICD-10 claims. “Physicians who are not compliant are going to see this in their bottom line.” cautions Monestime. “Essentially, they will be providing free services.”
Since the codes are much more complex, training is key. Monestime shared a study that showed that “physicians expressed that their number one concern was with the documentation requirements associated with ICD-10.” ICD-10 codes express so much more, reflecting details of the health situation and its treatment. “That’s why training is so important,” Monestime states, emphasizing that it allows the clinician to really show the depth of the problem and the quality of care given to the patient.
The road to ICD-10 is not short, and a HIPAA-covered entity should be well on its way to getting prepared for the go-live date. Monestime maintains that at this stage providers should be well into “the last phase of the implementation stage, and getting ready for testing.” She continues that, by April, providers should be implementing training for clinicians and the entire staff, and that healthcare entities should practice using ICD-10 codes through the use of dual-coding and documentation well before the October 1 conversion date.
CREDIT
article by ERIKA ALDRICH