AdventHealth’s GRACE Helps With Early Detection of Breast Cancer
by REBEKAH PIERCE
October is Breast Cancer Awareness Month, and while we’ve known for many years that awareness and early detection can help save lives, it’s always been an “easier said than done” situation. Like many cancers, breast cancer is notoriously hard to detect and can be difficult to treat once it’s in the later stages.
As the most common cancer in women in the United States (except for skin cancer), breast cancer accounts for roughly 30% of all new female cancers each year. According to the American Cancer Society, about 42,250 women will die from breast cancer each year. There’s about a 1 in 8 chance that a woman will develop breast cancer, with incidence rates increasing by about 0.6% each year.
The good news is that breast cancer death rates have been steadily declining, at a rate of 42% since 2021. Much of this can be attributed to increased awareness and screening. If breast cancer is found early and is in the localized stage, the five-year relative survival rate is 99%, according to the American Cancer Society.
The problem? Historically, predicting breast cancer risk has largely been done based on age. Women between the ages of 40 and 44 have the option to start screening with a mammogram every year, but mammograms are only recommended on a yearly basis for women 45 and older.
Age is only one part of the equation, says Dr. Wesley Walker, Director of Genomics and Personalized Health at AdventHealth. Yet until now, that’s been the risk factor we pay the most attention to.
That’s all about to change thanks to GRACE.
What Is GRACE?
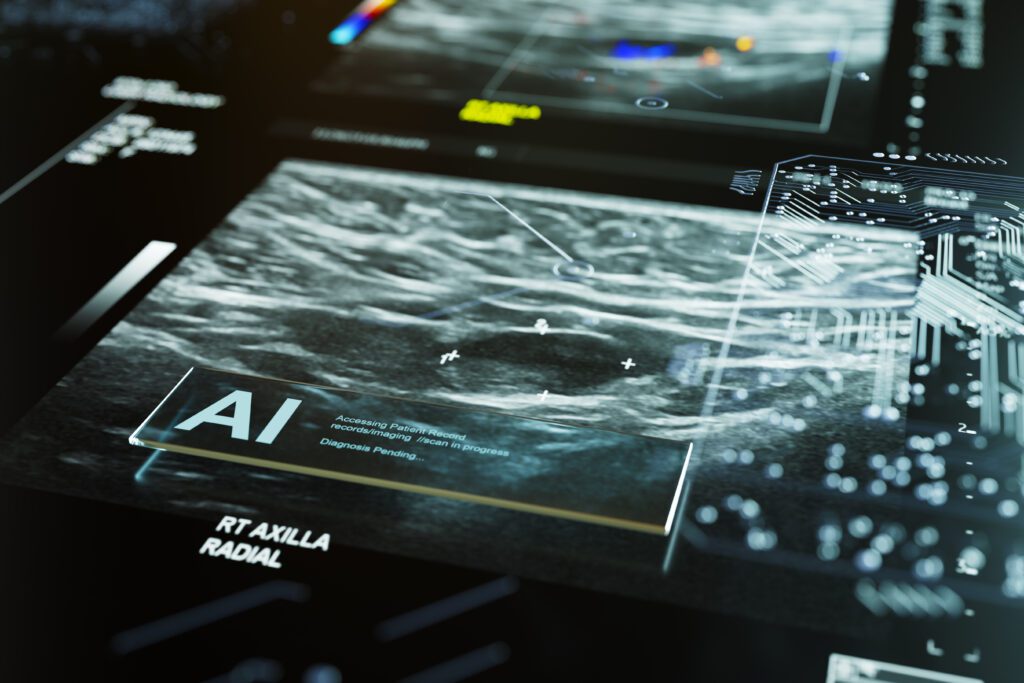
GRACE isn’t an actual person, but instead a tool that’s making a real impact on the lives of women across Central Florida. First conceptualized about one year ago, this AI pilot program was launched August 1 at two AdventHealth campuses — Winter Park and Waterford Lakes.
GRACE stands for Genomics Risk Assessment for Cancer and Early Detection, and is proving to be a powerful tool in the fight against breast cancer.
“The big idea behind the program is just to catch breast cancer early,” Walker says. “We know if we diagnose it early, when it’s small, and it’s treated, the patients do much, much better than if it’s found when it’s larger or even worse, if it’s spread to other tissues.”
It sounds like something out of a sci-fi movie, but the way GRACE works is actually quite simple.
“A person schedules a mammogram,” Walker explains. “Before they get it, they receive an electronic survey and fill out some additional questions. They get the mammogram, and that imaging goes into a software module that is AI-enhanced with image analysis. It basically predicts a density level that can have a big effect on their risk assessment.”
The “predicted density” is reviewed by a radiologist, who develops a finalized density before the information is entered into the risk assessment software.
“There are embedded algorithms within the electronic medical record that help us compute the risk assessment,” Walker continues. “These use the most advanced models and algorithms to give us the most precise risk assessment.”
After the assessment is generated, patients move into one of two pathways: high risk, or average risk. A patient who is deemed high risk will be contacted by a nurse navigator. A person with an average risk will continue with a standard regimen of mammography. High-risk patients will work closely with the nurse navigator, along with their primary care physician or OB GYN, to get the necessary support.
The end goal, according to Walker, is to make sure patients don’t fall through the cracks.
“We make sure we’re there to support them,” he says. “Learning you’re at high risk can be very stressful, so our nurse navigators have experience in talking to women about that type of issue and what that means…really just providing support along the way.”
The Future of AI in Healthcare
As our world relies increasingly on AI-driven solutions, it’s important to recognize that tools like GRACE hold immense value not just for patients, but for practitioners. “Physicians are extraordinarily busy people,” Dr. Walker expresses. “Time poverty is a fact of life for them. Anything we can do to facilitate the most advanced and precise risk assessment method and make it easy for this all to occur during a normal visit – they appreciate it.”
GRACE is proving to be useful not just in the early detection of breast cancer, but other cancers as well. The algorithm can also calculate the risk of Lynch syndrome, an inherited genetic disorder that is tied to an increased risk of developing certain cancers, like colorectal cancer. The concept works exactly the same, but the idea is to catch other types of cancer earlier, when they’re easier to treat.
“This really represents Advent Health’s work to personalize and individualize care in an evidence-based way,” Walker says. “This work will only become more progressive and important as time goes on. We’re moving from a one-size-fits-all to a truly more personalized approach.”
The plan is to introduce GRACE to an additional 16 sites around Central Florida in 2025, but Walker has an even broader vision than that.
“Increasingly, we are adapting AI to health care and need to do so,” he explains. “Advent Health is very involved in that effort. These tools are going to become standard in medicine.”