Do You Know What Migraine Really Is?
by TIM CRAIG
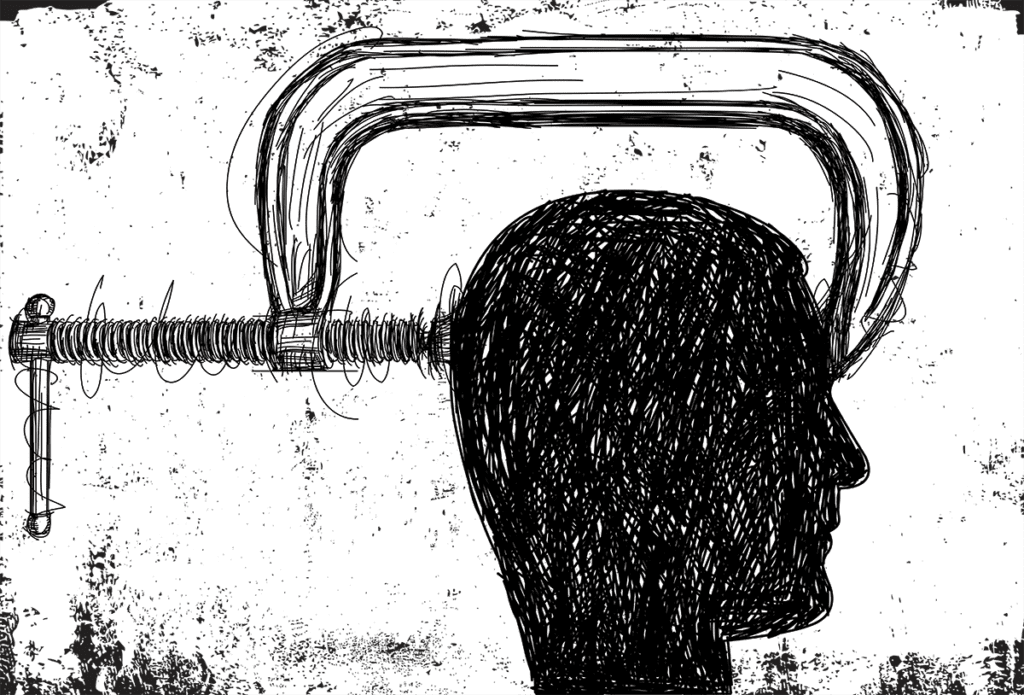
“It kind of feels like a vice grip on my head, almost similar to feeling like your head’s being stabbed.”
Amy Beatty is describing what her typical migraine feels like. Beatty, from Winter Haven, has been getting migraines since she was 16. Now, the librarian and mother of two recognizes when a migraine is around the corner.
“For me, when I start to get visual disturbances, like colors or bright lights in my field of vision, I know there is going to be pain within the next couple hours,” she says. “Sometimes the trigger is that there’s an extra amount of energy about a day before and I feel like I’m moving really fast.”
Beatty is one of 39 million Americans — and over a billion worldwide — who suffer from migraines. June is National Migraine and Headache Awareness Month, but still, migraine is an often-misunderstood condition that is the third-most-prevalent illness in the world.
Migraine or Headache: What’s the Difference?
Headaches are classified into two main groups: primary, which refers to independent conditions that cause pain in the head, and secondary, which occur as a result of another condition. Primary headaches include tension headaches. Secondary headaches are ones that come as a part of another condition, like a sleeping disorder or inflammation.
A migraine is typically thought of as a severe headache, but headaches are only one symptom of migraine. A migraine is a neurological condition that involves nerve pathways and chemicals. Changes in brain activity affect blood in the brain and surrounding tissues, causing a range of symptoms including nausea, sensitivity to light, dizziness, and extreme fatigue. Other more disruptive symptoms include visual disturbances, cognitive impairment, muscle weakness, and transient aphasia (difficulty communicating, verbalizing and finding words).
A migraine usually affects one side of the head (though not always), and according to the American Migraine Foundation, there are four distinct phases to a migraine. Again, because each individual’s experience is unique, not everyone experiences every phase.
- Phase I: Prodrome — Also known as “pre-headache,” this phase can last several hours or can even last several days. Symptoms in this phase include fatigue, sensitivity to light and sound, nausea, frequent yawning and frequent urination.
- Phase II: Aura — An estimated one-third of people experience this phase, during which people can experience blurry vision, episodic vision loss, flashing or “zig-zag” lights. These symptoms last anywhere from five minutes to an hour.
- Phase III: Headache — This phase is distinguished by severe or debilitating pain on one or both sides of the head that can last from several hours to several days. Along with the pain, other symptoms in this phase include anxiety; hypersensitivity to light, sounds, and smells; nausea and vomiting.
- Phase IV: Postdrome — Also called “migraine hangover,” this phase follows the period of pain and can last 24 to 48 hours. It’s characterized by fatigue, body aches, dizziness and difficulty concentrating. For some people, postdrome can be just as debilitating as Phase 3.
Migraine Triggers
Triggers range from environmental to hormonal to behavioral. Some environmental behaviors include bright lights, weather changes, particularly changes in barometric pressure and hotter temperatures. Behavioral triggers can include alcohol — particularly red wine — caffeine, cheese, processed meats and dehydration. Hormonal changes include fluctuations in estrogen levels, which could explain why migraines disproportionately affect women.
Identifying triggers is the single, most important step in treating migraines. Once identified, the triggers can be avoided or minimized to decrease the number and severity of migraine episodes. Doctors can provide resources, and there are a number of websites and social media groups for migraineurs that help in sharing coping advice.
Treatment
There are a variety of treatments for migraines, but they usually fall into two categories: abortives, which help relieve pain once a migraine has started, and preventives. Relief medications work best when taken at the first sign of an oncoming migraine. These include over-the-counter or prescription pain relievers; triptans, which are prescription drugs that block pain pathways in the brain; and other medications focused on lessening the effects of nausea, light and sound sensitivity.
Preventive medications are aimed at reducing how often patients get a migraine and how long they last. These include blood pressure-lowering medication, beta-blockers, anticonvulsants, antidepressants, Botox injections, and once-a-month monoclonal antibody injections.
For patients with migraines that do not respond well to medications or therapies, an alternative option is neurostimulation.
Many doctors recommend biofeedback, which includes muscle relaxation and abdominal breathing techniques that have been proven to reduce headaches and improve the quality of life for migraineurs. Many times, this treatment is paired with preventive medication.
Migraine and Dementia
Findings from a 2020 study published in the Journal of Headache and Pain supported the hypothesis that migraines are a midlife risk factor for dementia later in life, based on the higher rate of dementia in individuals with a hospital-based diagnosis of migraine with aura. The study also noted that further study should be conducted, particularly among populations with less severe migraine cases.
Coping Together
It’s important that family and friends understand the importance of their support and management. Understanding the condition and not downplaying migraine or its symptoms help the migraineur get the treatment and accommodations they may need.
Beatty says that in a family, an active migraine episode affects all parts of family life. Making sure the family knows what is happening and can adapt is key.
“Believe me, I would much rather be doing the daily family routines than have a migraine,” she says. “It’s important that the person who is suffering from the migraine does not feel that additional stress.”