Man’s Experience Underscores Importance of Advocating for Yourself as a Patient
by TERESA SCHIFFER
No one knows your body better than you. There may be times when something just doesn’t feel right, and even though you voiced your concern to your physician, you weren’t able to get the answers that put your mind at ease. As Roger Walker can tell you, this is no time to silently accept your fate and wait for “something” to happen.
“I started to feel pressure on my chest when I was working outside in the yard cutting the grass or whatever,” Walker says. “It kind of came and went, came and went, no big deal. But then it became more frequent and longer-lasting. At that point, I went to my primary care physician and they did a bunch of tests.”
The doctor ran a number of standard tests, but the only thing that showed up was a heart murmur that Walker was not previously aware of. Other than that, no issues were found. He was then referred to a BayCare cardiologist. More tests were performed, but again, no problem was found.
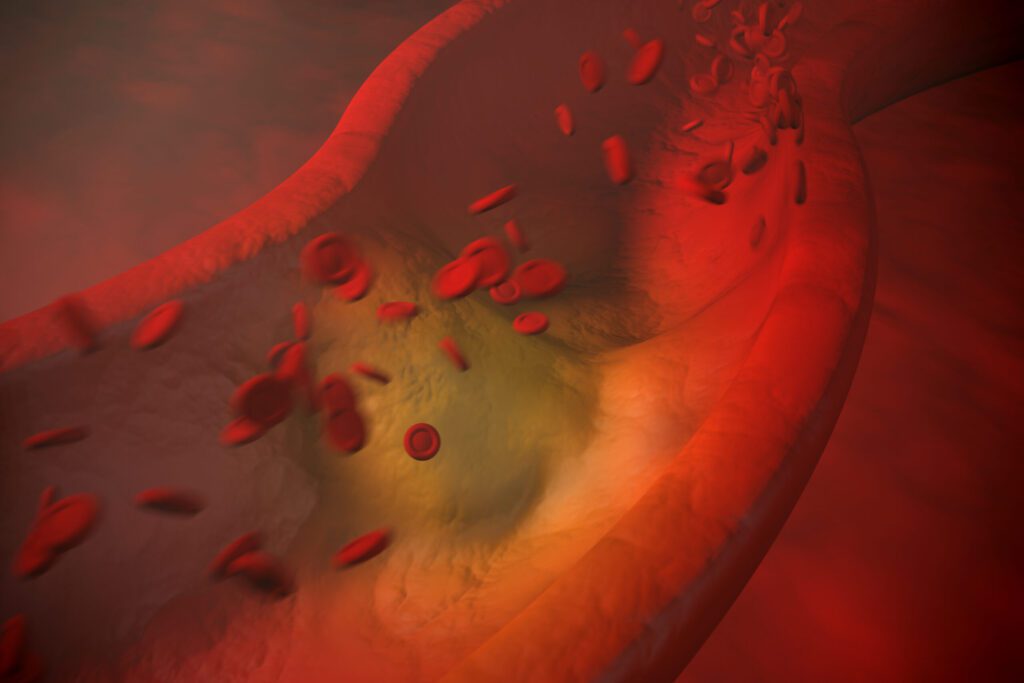
Two options were then presented to Walker: He could simply wait and see what happened, or he could undergo cardiac catheterization for a deeper analysis of what was happening inside his body. During this process, a thin, flexible, hollow tube (the catheter) is inserted into a blood vessel. The catheter is then threaded through the blood vessel into the aorta, where it can be used to check the pressure within the chambers of the heart and other diagnostic procedures.
“Well, I’m 78 years old,” Walker told the doctors, “The problem’s not going away. I think we ought to do the heart cath.”
On August 10, Walker, an avid golfer, underwent the cardiac catheterization procedure at BayCare’s Winter Haven Hospital. He was told that one of three scenarios was likely: they would find nothing, they would find something they could deal with right away by putting in a stent, or they would find a significant enough blockage to warrant open-heart surgery.
When he awoke after the procedure, Walker was told that his right coronary artery was found to be 99 percent blocked, and a stent was put in place at that time in order to open up the artery. The timing could not have been any more fortuitous – the next day, all such procedures were halted due to the surge in COVID cases caused by the delta variant. This meant that the Outpatient Rehabilitation Center was also closed, so Walker would be unable to start rehab right away.
Almost three months passed before Walker could begin heart rehab at BayCare. During that time, he stayed active by playing golf, doing yard work, going to the gym, and engaging with his church and community.
Walker recognizes the benefit his active lifestyle has had on his recovery.
“I’m a very active person, so I stayed busty. I cut a few lawns, I played golf, I did a lot of different things with my church and the city. Right now, I’m a ranger at the golf course – I was up there for seven hours today. Because I was doing that, I was doing different things every day, I wasn’t sitting in my chair wasting away.”
This helped mitigate the delay in starting his rehab. On November 5, Walker finally was able to start the first of 36 sessions with the wellness center. Rehab consists of three visits per week to the Outpatient Rehabilitation Center. During each hourlong visit, Walker is monitored as he works his body with different apparatuses.
He describes a typical rehab session, “I do four different stations within that hour, and they’ve steadily been building up the amount of watts that they’re using and the amount of time that I’m using it. So when I started, each session was about six to eight minutes at the lowest level. Now, on one of the machines, I’m at 35 watts and I’m doing it for 11 minutes. So I do a warm-up drill, then I do the four apparatuses, and then I do a cool-down period. They take my blood pressure when I start, and then after the apparatuses and the rest time.”
Now that he is roughly two-thirds of the way through the prescribed rehabilitation process, Walker is feeling a lot better and no longer experiencing the severe pressure in his chest that was caused by the blockage.
“I’m fine,” Walker tells us. “I’m not having any issues at all.”
At the end of the day, only you know what is normal for your body. When something feels “off,” talk to your primary care physician right away. Sometimes, the initial tests won’t reveal the underlying issue immediately. When this is the case, continue to request follow-up care and more testing. Be persistent when necessary. Don’t wait for a serious problem to emerge before taking action. By then, it could be too late.
“You don’t need to wait until something happens,” Walker advises. “You need to be proactive.”