Virus Changes How Clinics Reach Patients
by TIM CRAIG
It didn’t take long for Central Florida Health Care CEO Ann Claussen to realize that the COVID-19 virus was going to change the way they do things.
Claussen says that in early March, Polk County’s first confirmed case of the virus was diagnosed through the group’s Dundee clinic. “From that very first test, we put all the measures in place and immediately put heightened awareness procedures for the safety of all our staff and our patients,” she says.
In addition to the safety measures, Claussen enacted “overcommunication” protocols to CFHC’s 13 clinics in Polk, Highlands and Hardee counties. “We wanted to make sure we were doing everything right,” she says. “We were on alert with the CDC and the leadership team was meeting at least twice a day to make sure we were all working with the same information.”
Communication is important because of the unique patient population CFHC serves. The clinics are federally qualified health centers, which means they treat everyone — the uninsured and underinsured patients as well as those with Medicaid, Medicare, and insurance. There are 11 clinics in Polk County, as well as one each in Avon Park and Wauchula. The clinics offer a wide array of services, including medical, dental, OB/GYN, pediatric and mental health. There are eight pharmacies within the clinics. Last year, the group treated 55,690 patients and had 228,201 visits. The 13 clinics employ 440 medical and professional staff.
However, once the virus hit, things changed. The biggest change was stopping all of the well visits and regular exams. Staff was sent home for paid time off. It was during this time, the focus was on keeping everyone healthy … but there was another challenge that Claussen and the leadership team wanted to tackle.
“During that time, we tried to figure out how to do things different,” she says. “How can we take the resources we have and still serve our patients and still keep everyone safe?”
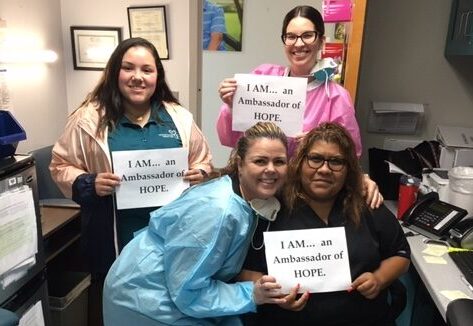
The answer: Reach out instead of take in. “We were trying to think outside the box,” she says, “and we wanted to involve our staff as much as possible.”
The result was the first of many outreach projects, dubbed COVID-Silver
“The COVID-Silver Project brought together our case managers and our Navigator staff to individually call all of our 65-and-older clients,” says Claussen. “We wanted to ask if they needed refills on their medication or if they needed any food and those kinds of things. We just wanted to let them know that we were here and haven’t forgotten about you.”
The response was overwhelmingly positive and impactful, particularly for one patient.
“We were reaching out and asking questions and one of our patients noted that they were not feeling that well,” says Claussen.
The patient described what they were feeling to the case worker, who was concerned enough to bring in a physician. The physician told the patient to come to the clinic right away.
“It turned out the client was having a heart attack and we were able to get her to the hospital,” says Claussen. “She is going to be fine, but she was sitting at home having a heart attack and not sure what to do. We were able to help her.”
The success of the COVID-Silver project led the clinic to start others — COVID-Grin focuses on dental care, with the clinics open for emergency care. Staff also calls OB and diabetic patients to discuss health education and oral health. COVID-Mind focuses on behavioral health and phone counseling.
“When patients stay at home, it can become difficult for them to connect with others,” says Claussen. “This is a way to help maintain mental health for the patient and a continued connection for us.”
The clinics also host parking lot COVID testing at some locations. People who think they may have the virus are examined to see if they are presenting symptoms and then tested — without leaving the car. Four to eight days later, says Claussen, the test results come back and the patients are notified.
Telehealth and telemedicine efforts have also increased, including the clinic’s first tele-dental visit, in which a patient who was having post-surgery discomfort shared a photo of the troubled area and a video chat with the doctor. “It resulted in the patient getting prescribed additional antibiotics until they can come to the clinic,” says Claussen.
Claussen says that all of these new programs and outreach efforts have made her realize that this could be a new path for the clinic as a whole.
“It made us realize how important reaching out is now,” Claussen says.
“And it also made us realize that once life comes back to normal, there are some of these things that we want to continue to do.”