In the June article, we discussed aortic dissection, its symptoms, and its classification. Let’s discuss other aspects now.
Aortic dissection is most commonly diagnosed when the patient presents with tearing chest or back pain that is unrelenting and associated with severely elevated blood pressure. Other signs indicative of various important organs not getting enough oxygen/blood flow to them may be associated with this presentation like leg ischemia, cardiac tamponade, and mesenteric ischemia.
Aortic dissection is most commonly diagnosed with a computed tomography angiogram scan, which is often done in an emergency room. This scan involves contrast dye that is injected through a peripheral intravenous cannula.
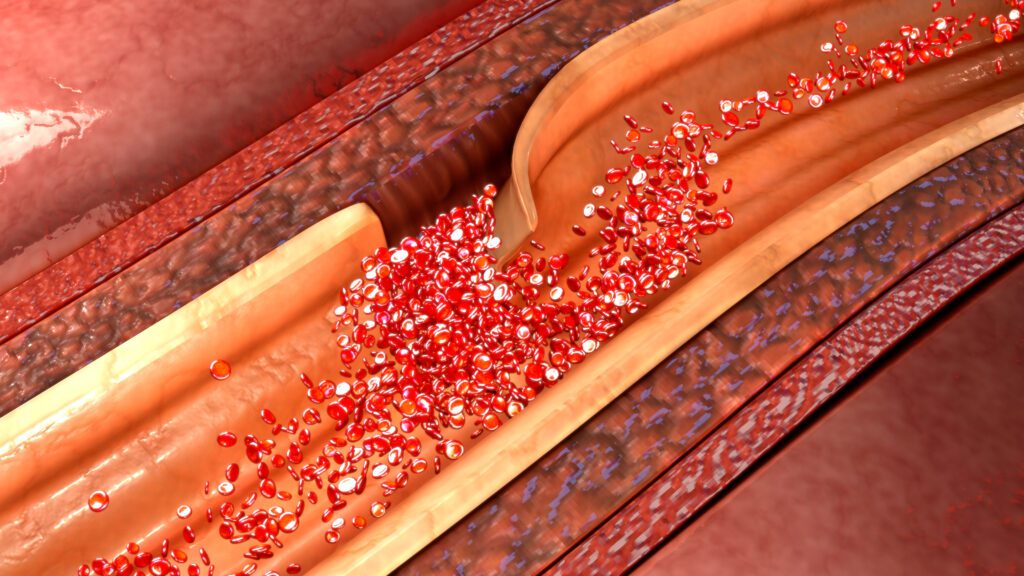
Stanford Type A aortic dissections are generally managed surgically. Stanford type B aortic dissections are typically managed by controlling the systolic blood pressure to less than 120 mm Hg and the heart rate to less than 60. Patients usually need to be monitored very closely in the intensive care unit and they may need multiple fast-acting intravenous drips to lower the blood pressure if needed. If symptoms do not respond to this treatment, surgical management may be needed. Thoracic endovascular aortic repair (TEVAR) is a procedure that involves placing a stent graft in the true lumen of the thoracic aorta to improve the amount of blood supply to the important organs in the body.